Introduction
Mast cells are long-lived tissue-resident cells with an important role in many inflammatory settings, including host defense against parasitic infections and allergic reactions. They are part of the body’s first line of defense and are involved in various physiological processes, including inflammation, wound healing, and defense against pathogens. They are distributed around the microvascular endothelium in the oral mucosa and dental pulp. Mast cells release a variety of preformed and newly formed physiological mediators. Their mediators play a significant role in tissue damage and propagation of inflammatory responses. Let us discuss the role of these cells in periodontal disease pathogenesis in detail.
Origin and Development
Mast cells originate from hematopoietic stem cells in the bone marrow. These stem cells differentiate into mast cell precursors, which then migrate to various tissues throughout the body where they mature. Unlike other blood cells, mast cells are not typically found in the bloodstream; instead, they reside in tissues, particularly those that are in close contact with the external environment, such as the skin, respiratory tract, and gastrointestinal tract. Unlike other white blood cells, mast cells are released into the blood as mast cell progenitors and do not fully mature until they are recruited into the tissue where they undergo their terminal differentiation. During this process, several factors play a crucial role, including stem cell factor (SCF), which is essential for mast cell development, proliferation, and survival. Once in the tissue microenvironment, mast cells complete their maturation and become fully functional players in the inflammatory response. These cells exist in three distinct forms based on their structure:
Intact cells: Mostly found in blood vessels and dermal tissues. Granules are closely packed together, obscuring other cellular organelles.
Spreading cells: Occur in superficial connective tissue. These cells have fewer granules than intact cells.
Degranulated cells: Result from the release of granules during immune responses.
Structure and characteristics of mast cells
Mast cells are characterized by their large size and the presence of numerous granules within their cytoplasm. These are mononuclear cells consisting of small secretory granules that range in size from 0.2 to 0.8 micrometers. In some cells, the granules are dense enough to obscure the appearance of the nucleus. The cells are oval or irregularly shaped with a single central nucleus. Within the nucleus, densely packed peripheral chromatin can be observed. Most of the cytoplasm is occupied by cytoplasmic granules, but there are also a few secondary lysosomes. Additionally, mast cells have small, finger-like projections from the cell membrane. The plasma membrane of mast cells contains IgE receptors. These receptors bind to the Fc region of circulating IgE antibodies. Binding of IgE antibodies induces degranulation of mast cells, releasing their stored mediators. When mast cells are activated, they release these substances through a process called degranulation. The chemical mediators released from mast cells can be divided into two categories,
Preformed Mediators (Stored in Granules):
These preformed mediators are stored in large granules within the mast cell cytoplasm. These are rapidly released upon cell stimulation:
Histamine: It is one of the most well-known mediators released by mast cells. It plays a key role in allergic reactions and is responsible for many of the symptoms associated with allergies, such as itching, swelling, and redness. Histamine acts by binding to histamine receptors on various cells, leading to increased vascular permeability, smooth muscle contraction, and stimulation of nerve endings.
Neutral proteases: Enzymes that break down proteins. Proteases, such as tryptase and chymase, are enzymes that break down proteins and play a role in tissue remodeling and defense against pathogens.
Heparin: It is an anticoagulant that helps to prevent blood clotting. In mast cells, heparin is stored in the granules and released upon activation. It plays a role in modulating the immune response and maintaining tissue homeostasis.
Chondroitin sulfate: A component of connective tissue. While heparin is the predominant glycosaminoglycan (GAG) associated with mast cells, they also produce other GAGs, including heparan sulfate and chondroitin sulfate.
De Novo Synthesized Mediators (Produced After Activation):
These mediators are synthesized only after mast cell activation:
Leukotrienes (LTB4, LTD4): Involved in inflammation and immune responses.
Prostaglandin D2 (PGD2): A potent vasodilator.
Platelet-activating factor (PAF): Regulates platelet aggregation and inflammation.
Cytokines: Including IL-10, IL-8, IL-5, IL-3, IL-1, GM-CSF, TGF-β, VEGF, and TNF-α3
Mast Cell Disorders
While mast cells are essential for normal immune function, their dysregulation can lead to various disorders. Some of the most common mast cell disorders include:
Mastocytosis
Mastocytosis is a rare condition characterized by the abnormal accumulation of mast cells in various tissues, including the skin, bone marrow, liver, and spleen. It can present in different forms, ranging from a relatively benign cutaneous form (limited to the skin) to a more aggressive systemic form that affects multiple organs. Symptoms of mastocytosis can include skin lesions, gastrointestinal symptoms, and anaphylactic reactions.
Mast Cell Activation Syndrome (MCAS)
MCAS is a condition in which mast cells are overly sensitive and prone to inappropriate activation, leading to the excessive release of mediators. This can result in a wide range of symptoms, including allergic-like reactions, gastrointestinal issues, cardiovascular symptoms, and neurological manifestations. The diagnosis of MCAS can be challenging due to the variability of symptoms and the lack of specific diagnostic tests.
Allergies and Anaphylaxis
Mast cells are key players in allergic reactions and anaphylaxis, a severe, potentially life-threatening allergic reaction. In individuals with allergies, mast cells are sensitized to specific allergens through the binding of IgE antibodies. Upon exposure to the allergen, these sensitized mast cells rapidly degranulate, releasing large amounts of histamine and other mediators that cause the symptoms of an allergic reaction. Anaphylaxis requires immediate medical attention and is typically treated with epinephrine.
Role of mast cells in immune response against periodontal pathogens
Mast cells play a significant role in the pathogenesis of periodontal diseases. Periodontal cells and inflammatory-immune cells, including mast cells (MCs), produce cytokines and chemokines. These mediators contribute to local inflammation within the gingival tissues. Let us discuss the role of mast cells in immune response in periodontitis,
Inflammatory Response
Periodontitis is characterized by a complex inflammatory response to the bacterial biofilm that forms on the teeth. Mast cells, as key players in the immune system, are among the first responders to bacterial invasion. They are found in increased numbers in the gingival tissues of patients with periodontitis compared to healthy individuals. These cells contribute to both the initiation and progression of periodontal inflammation through the release of various mediators.
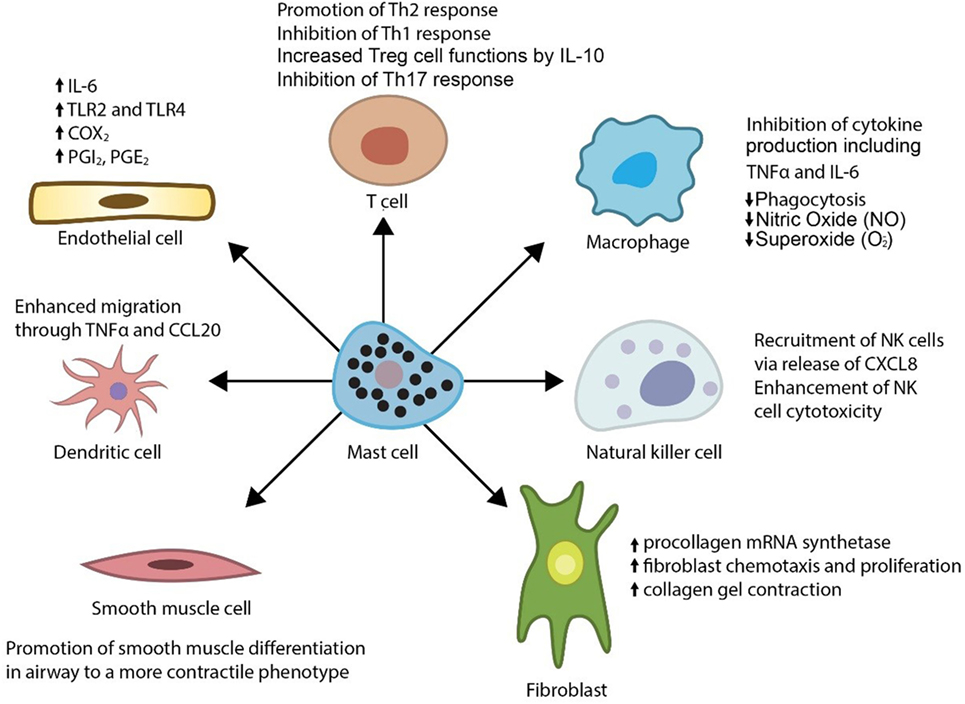
Interaction with Other Immune Cells
Mast cells interact with other immune cells, such as T cells, B cells, neutrophils, and macrophages, to coordinate the immune response. For example, they can present antigens to T cells, thereby influencing the adaptive immune response. Mast cells also release mediators that can modulate the activity of these immune cells, further amplifying the inflammatory response in periodontitis.
Tissue Destruction and Bone Resorption
One of the hallmarks of periodontitis is the destruction of the periodontal ligament and alveolar bone. Mast cells contribute to this process through the release of proteases and other mediators that degrade the extracellular matrix and bone. Histamine and other vasoactive substances released by mast cells increase blood flow and vascular permeability, facilitating the migration of osteoclast precursors to the bone surface, where they differentiate into active osteoclasts and resorb bone.
Angiogenesis
Mast cells also play a role in angiogenesis, the formation of new blood vessels, which is a critical component of the inflammatory response in periodontitis. They release angiogenic factors, such as vascular endothelial growth factor (VEGF), that promote the growth of new blood vessels. This process ensures an adequate supply of nutrients and oxygen to the inflamed tissues, but it can also contribute to the persistence and progression of inflammation.
Clinical Implications
Diagnostic Potential
The presence and activity of mast cells in periodontal tissues could serve as a potential diagnostic marker for the severity and progression of periodontitis. By assessing the levels of mast cell mediators in gingival crevicular fluid or tissue samples, clinicians may be able to better understand the inflammatory status of the periodontium and tailor treatment accordingly.
Therapeutic Targeting
Targeting mast cells and their mediators offers a promising approach for the treatment of periodontitis. Some potential therapeutic strategies include:
Mast Cell Stabilizers: Medications such as cromolyn sodium can prevent mast cell degranulation, reducing the release of inflammatory mediators.
Antihistamines: These drugs can block the effects of histamine, reducing vascular permeability and inflammation.
Protease Inhibitors: Inhibiting mast cell proteases, such as tryptase and chymase, can help to prevent tissue destruction and bone resorption.
Cytokine Inhibitors: Targeting specific cytokines released by mast cells, such as TNF-α or IL-6, can reduce inflammation and tissue damage.
Combined Therapies
Given the multifactorial nature of periodontitis, a combination of therapies targeting different aspects of the disease may be most effective. For example, combining antimicrobial treatments to control the bacterial infection with anti-inflammatory therapies targeting mast cells and other immune cells could provide a comprehensive approach to managing periodontitis.
Conclusion
Mast cells play a critical role in the pathogenesis of periodontitis through their involvement in the inflammatory response, tissue destruction, and bone resorption. Understanding the mechanisms by which mast cells contribute to periodontitis can lead to the development of targeted therapies that may improve treatment outcomes and reduce the burden of this common and debilitating disease. As research continues to uncover the complex interactions between mast cells and other components of the immune system in periodontitis, new diagnostic and therapeutic strategies will likely emerge, offering hope for better management of this condition.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:

